Longo surgery to treat haemorrhoids
Longo surgery is procedure to treat advanced, stage III-IV haemorrhoids. During the procedure, the excess mucosal cylinder causing the prolapse is removed by circular excision on the mucosa of the last section of the rectum.
What is a haemorrhoid and why does it develop?
The rectum, which is interwoven with a fine vessel and neural network, and the mucous membrane that covers it, is one of the most sensitive areas of our body. The vascular network that weaves through it, as well as the vascular cushioning, play an essential role in the proper functioning of the rectum, as these so-called arteriovenous vascular cushions have the task of providing a hermetic seal to the rectum in all three directions. These vascular cushions also include circularly located varicose veins, as well as haemorrhoids.
We can talk about haemorrhoid disease when the vascular network dilates and the connective tissue that secures the vascular pad stretches. The walls of the veins in this case become thinner and more vulnerable, eventually slipping through the anus with the stagnant blood in them due to their weight, and the haemorrhoids are trapped between the rectum’s sphincter.
The most common cause of haemorrhoids is connective tissue weakness, which is hereditary, therefore if you have a history of haemorrhoids in your family, you should pay close attention to your symptoms. Strain during defaecation, pressure on the pelvic veins in women during pregnancy can be a direct cause, and a sitting, sedentary lifestyle, low-fibre diet, and obesity can greatly contribute to its development.
The developed hemorrhoidal disease is an irreversible condition, without treatment it gradually gets worse and serious complications can develop.
What are the symptoms and stages of haemorrhoids?
Haemorrhoids often do not cause symptoms for quite some time. Later, however, after defecation, the dilated veins may bleed, drawing a streak of blood on the stool or toilet paper. The bleeding is not painful, the amount is usually small.
At a more advanced stage, protrusion of the hemorrhoidal nodules can also be observed around the anus. The pain usually occurs when defecating, but it does not disappear completely afterwards, an uncomfortable, straining, stinging feeling may remain, which can also be a problem when sitting. The surface of the nodule on the outside may rub and become a wound and produces discharge.
However, it is important to point out that these symptoms can also be caused by other rectal diseases (inflammation, rectal polyps and fistulas, etc.), therefore it is recommended to consult a proctologist as soon as possible.
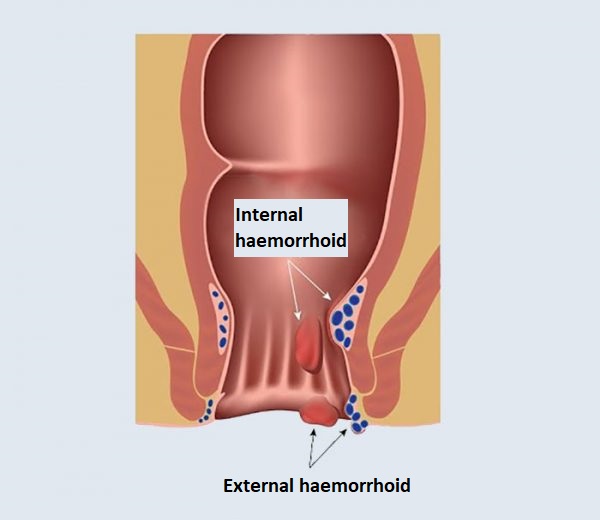
When it comes to haemorrhoids, we distinguish between external and internal haemorrhoids. The haemorrhoid that forms on the outer, skin-covered part of the rectum is called the outer haemorrhoid, and the haemorrhoid that forms on the inner, mucosal lining of the rectum is called the internal haemorrhoid. The exact type of haemorrhoids can be determined by a proctologist after colonoscopy.
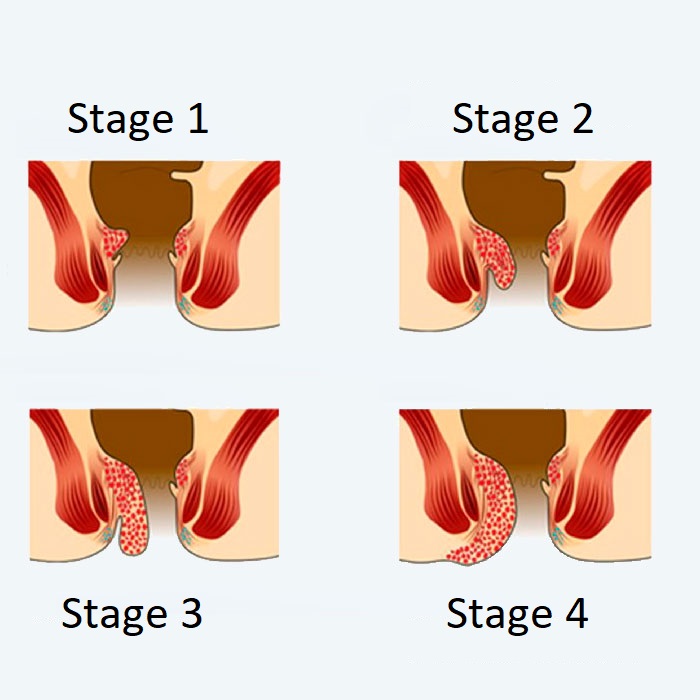
In the case of internal haemorrhoids, 4 stages are distinguished depending on the size and progression of the nodules. However, these stages do not necessarily reflect the severity of the patient’s complaints.
stage 1: the nodules may bleed, but there is no prolapse or pain
stage 2: under increased pressure (defecation), the vascular nodule prolapses but recedes spontaneously
stage 3: in case of abdominal compression, defecation, the nodules prolapse and can only be placed back with the help of the fingers
stage 4: the blood vessels are bent, making it impossible to empty them, acute pain occurs, the haemorrhoid nodules are excluded
When is Longo surgery recommended?
Minor haemorrhoidal complaints are treated conservatively using ointments, suppositories, lifestyle, and dietary changes, and in the case of larger nodules, a rubber ring. If treatment is ineffective and symptoms persist for a long time, surgical treatment may be recommended.
In case of advanced, stage III and IV internal haemorrhoids, surgery is recommended in all cases. In addition to the conventional surgical procedure, in such cases, if a large circular prolapse of the mucosa and the haemorrhoid nodules, is observed, then Longo surgery, i.e. circular mucosal excision, can be an effective solution.
What happens during Longo surgery?
During the preoperative consultation, the proctologist will provide detailed information about the necessary preoperative tests, as well as the course of the surgery and its risks.
The surgery is performed under general or spinal anaesthesia. During the procedure, the specialist uses a special circular suturing machine (PPH machine) to cut a cylinder out of the rectal mucosa to eliminate the progression, and at the same time creates a series of sutures to unite the tissues. During the operation, the sensory skin surface is not affected and no skin damage occurs.
During the procedure, the tissue causing the prolapse of the haemorrhoids and rectal mucosa excess will be excised, the arteries feeding the varicose veins will be intersected. As a result, venous outflow improves, blood vessels are emptied, and the internal and external haemorrhoids wither, and excess tissue is eliminated.
The duration of the surgery is 20 minutes.
What are the advantages of the procedure?

The biggest advantage of the procedure compared to conventional haemorrhoid surgery is that no skin damage occurs during the surgery, thus minimizing post-operative pain, shortening the length of hospital stay, and healing time, allowing the patient to return to work and normal life in a short time.
What are the risks of the surgery?
Like all medical interventions, Longo surgery can have risks and complications. After the procedure, bruising around the rectum, watery, swelling or inflammation of the small skin appendages may occur. Rarely, inflammatory complications, which can be prevented by giving the patient antibiotics, may occur.
What can I expect after the surgery?
In the hours following surgery, minimal rectal pain may occur, which is relieved with an injectable analgesic. The next day after the surgery, this pain is minimized and even disappears. This is when the first defaecation is expected, which may not cause pain but minimal bleeding. On the second day after surgery, the patient can leave our hospital.
In the days after surgery, bruising around the anus, milder swelling, inflammation may occur. In the week following the operation, with the relief of the complaints, the physical exertion can be increased, however, strong physical exertion, sports, long-term sitting, and abdominal press are allowed only later.
To maintain the consistency of the stool, supplementing the usual diet with fibrous foods and plenty of fluids is recommended.
What is included in the price of our surgeries?
- costs of the surgery
- costs of anesthesia (local or general anesthesia, postoperative pain relief)
- the costs of the planned hospital stay and care
- necessary medicines and certain medical aids during the stay
- inpatient physiotherapy treatment (if necessary for rehabilitation)
- if necessary, the fee for the planned histological examination
- the price of the first follow-up examination
What additional costs might be expected?
- implants
- consultation with the anesthesiologist (must be done in Medicover)
- pre-operative examinations (if performed by us)
- in case of blood group antibody positivity, the blood matching fee
- hotel service fee for extra care days
- aids for further rehabilitation
- accompanying person staying in the hospital
- day (with one meal) 20 000 HUF
- night (full board) 60 000 HUF
- furthermore, if necessary, the cost of the 2nd follow-up examination is the fee of the specialist examination -50%, the cost of the 3rd follow-up examination is the fee of the specialist examination -30%
The course of the surgery
Before surgery
- pre-surgery specialist consultation, where the specific surgical proposal is made
- consultation with the Case Manager
- general information if necessary
- preparation of a written quotation
- booking surgery and preliminary examination appointments
- payment
-
carrying out pre-operative examinations
-
arrival for surgery
On the day of surgery
- arrival at Medicover Hospital at 6:30
- check-in at the reception on the ground floor
- occupying a room accompanied by a nurse, who provides information
- morning visit with the specialist physician and anesthesiologist
- surgery
- postoperative monitoring
- afternoon visit with the specialist physician
- constant anesthesiology specialist monitoring in the postoperative period
- discharge (with an accompanying person), final report and handing over a certificate
Surgical service process
- surgery
- hospital stay and care
- planned histology
- follow-up examination, sutur removal
