Anterior cruciate ligament (ACL) surgery
Anterior cruciate ligament injury is one of the most common types of knee ligament injuries that occur during sports activities. Injury to the cruciate ligament changes the kinematics of the knee and, as a result, can cause long-term degenerative changes (wear on the joint surfaces, meniscus injury) if left untreated. The following article describes in more detail the anterior cruciate ligament injury and possible treatments, as well as the procedures for anterior cruciate ligament surgery.
Where is the anterior cruciate ligament located?
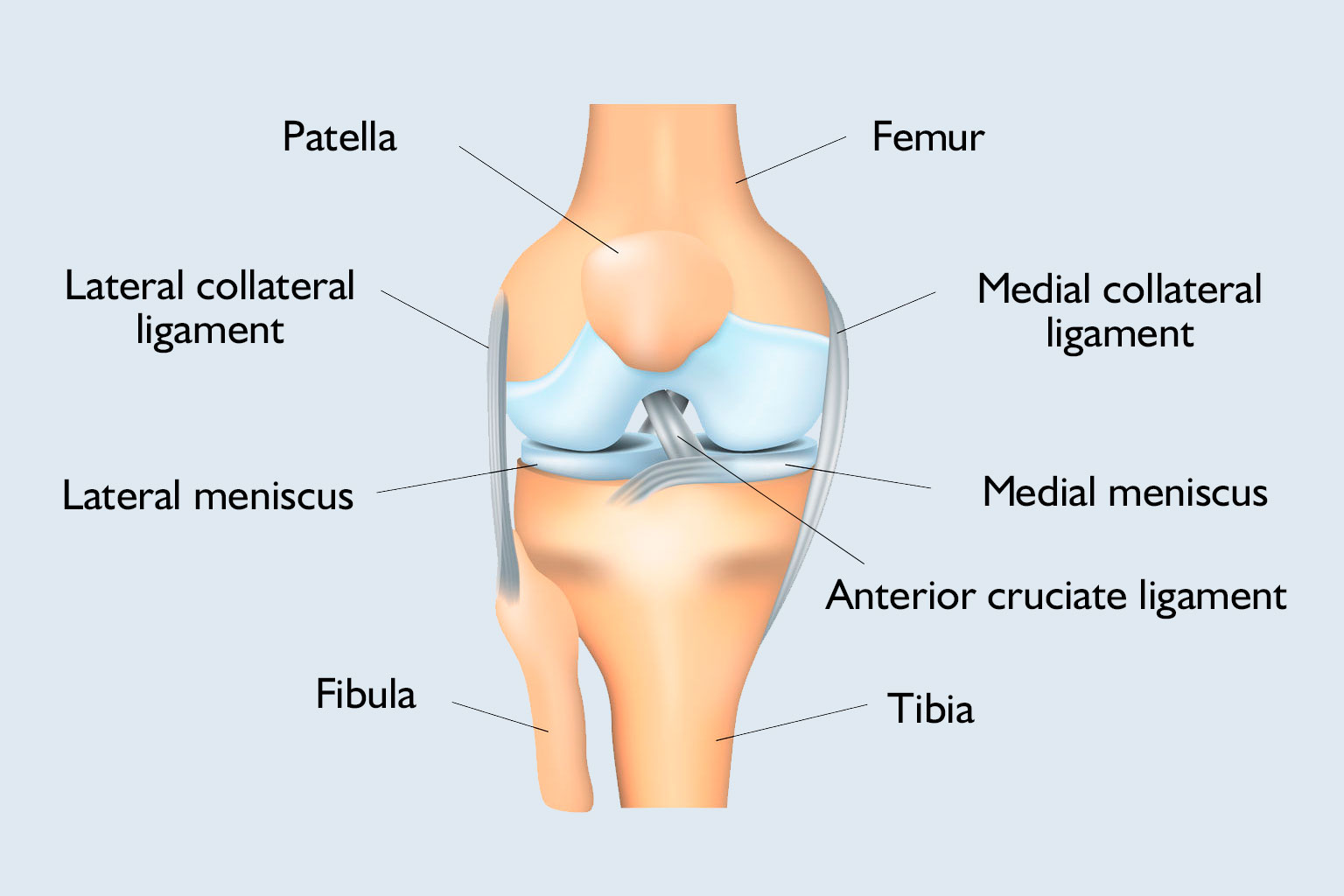
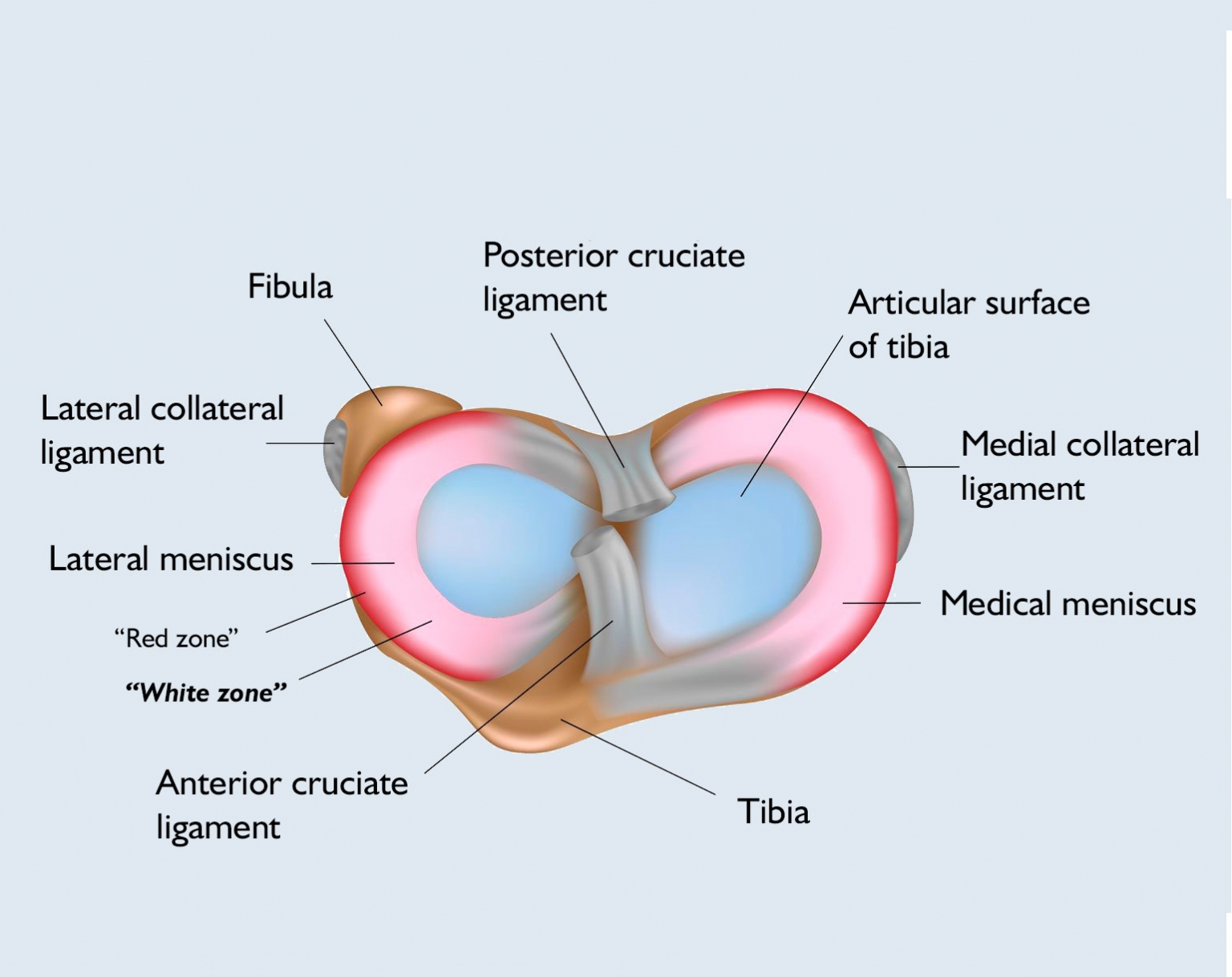
In addition to the tendons and muscles, four ligaments are responsible for the stability of the knee joint so that the bones do not move out of place: the lateral collateral and medial collateral ligaments prevent lateral movement, and the intersecting, anterior and posterior cruciate ligaments prevent forward and backward movement.
The anterior cruciate ligament (ligamentum cruciatum anterius – LCA) and the posterior cruciate ligament (ligamentum crutiatum posterius – LCP) are located in the middle of the knee, inside the joint capsule, and are covered with synovium. Bundles of fibres form both and due to the different location of the origin and adhesion points, one of the ligaments is always in a tight state.
The anterior cruciate ligament originates inside the condyle of the femur, twisting slightly outward about its own axis, moving forward, toward the midline, and adhering to the adhesion of the medial meniscus. Its length is approx. 30 mm, width approx. 10 mm and a thickness of approx. 5 mm. Heavy-duty measurements have shown that a force of 1800 N is required to tear the anterior cruciate ligament.
What is the function of the anterior cruciate ligament?
The anterior cruciate ligament performs the following functions within the knee joint:
- its primary role is to prevent the tibia and femur from moving forward during bending
- prevents excessive back bending (hyperextension)
- inhibits axial rotation of the knee
- acts as a secondary protection system against lateral forces
- twists the knee back to a stable position by tension in its fibres
How can the anterior cruciate ligament be damaged?
Injury to the anterior cruciate ligament (ACL) most commonly occurs during some form of sports activity, when the leg is twisted to an increased extent as the knee moves sideways. It is common among skiers and footballers, in case of irregular slips, or in handball players when the foot comes back at the wrong angle to the ground. In these cases, other formulas are often damaged in the knee, such as the ligaments or the meniscus.
What are the symptoms of anterior cruciate ligament injury?
In the case of an acute injury, a strong, snapping sound is heard at the moment of the injury, which is often heard not only by the injured but also by those close by. It is accompanied by severe pain, which causes the patient to feel their knee twisted out of place. The injury is also accompanied by a high degree of swelling, pressure sensitivity and limited mobility, and the injured person cannot step on the injured limb.
In the case of a chronic ACL tear, the patient’s knee feels unstable, protruding, and walking on uneven ground, climbing stairs, and rotational movements are accompanied with unsteadiness. In addition, long-standing anterior cruciate ligament injury also carries the potential for cartilage wear, injury of other ligaments and the meniscus, as the anterior cruciate ligament does not regenerate but slowly scars. This scarred tissue will no longer be able to perform the function of an intact cruciate ligament, it will have a loose, wavy course and thus lose its original, stabilizing role.

How is ACL tear diagnosed?
In case of injury to the knee joint, the traumatologist or orthopaedist first asks the patient about the circumstances of the injury and any previous injuries and surgeries, and then, if a cruciate ligament rupture is suspected, performs specific tests after the primary physical examination.
During the primary physical examination, the doctor assesses muscle mass, looks for any swelling, locates painful points by touch, and then examines the range of motion and the degree of instability.
If anterior cruciate ligament damage is suspected, the following specific tests can be used to determine the actual rupture:
- Lachman test: this test is best suited to detect anterior cruciate ligament rupture. The test consists of two components: the first one is the examination of the forward displacement of the tibia, in a loose, elongated, slightly twisted position, relative to the femur, because in the event of the rupture of the anterior cruciate ligament, the forward displacement increases. The other component is the examination of the hardness of the endpoint, which becomes soft when the anterior cruciate ligament ruptures. The most sensitive test, on the other hand, does not give reliable results with tense muscles or haematoma.
- Anterior drawer test: in this case, the doctor examines the forward movement of the tibia in a 90-degree bend of the knee joint. However, this test has a lower sensitivity and specificity for the anterior cruciate ligament than the Lachman test.
- Pivot shift test: with a bend of 30-40 degrees, with a slightly rotated position of the tibia, an outward turning force is applied to the knee joint. As a result, the tibia becomes sprained forward relative to the femur. With the knee slowly stretching, the tibia suddenly slides back into place at one point, a clear sign of an anterior cruciate ligament rupture. The disadvantage of the test is that it cannot be used in acute injuries due to pain.
If the tests do not give a clear result, knee arthroscopy may help determine the rupture of the ligament.
In the event of the rupture of the anterior cruciate ligament, imaging diagnostic procedures (MRI, ultrasound, X-ray) may only be required to assess and clarify possible secondary injuries (meniscus injury, collateral ligament injury).
How can an anterior cruciate ligament injury be cured?
Anterior cruciate ligament tear can be treated surgically or conservatively, and the knee specialist orthopaedist will decide if surgery is needed or the injury can be treated with physiotherapy and/or other conservative therapies.
Regardless of the extent of the injury, several factors affect whether conservative treatment is sufficient or if anterior cruciate ligament surgery is required. The patient’s age, physique, weight, physical activity and scope of activity are also important, as it does not matter for the subsequent load on the joint whether it is a lightweight individual, doing mostly sedentary job, or someone doing a standing job, or an athlete with strong physique. In the case of activities that significantly use the knee joint, ligament replacement is definitely recommended, but in case of less use, conservative therapy can also be used.
In case of both treatments, the primary goal is to restore knee stability.
Conservative treatment is recommended if the tear is less than 50%, the pivot shift test is negative, and the patient has no sense of instability. With the reinforced thigh muscles during the treatment, and by creating ideal load conditions, later surgery can be avoided, however, there is a risk of wear. The treatments also aim to restore painless movement, full range of motion and prepare for the increased load that can be achieved with special physiotherapy. Chilling can also be used as a supplementary treatment to reduce inflammation and pain.
During anterior cruciate ligament surgery, the torn cruciate ligament is replaced, the aim of which is not only to restore stability but also to prevent degenerative processes (meniscus injury, arthrosis). Anterior cruciate ligament surgery is recommended if the patient has a high activity lifestyle, a rupture greater than 50%, or meniscus injury and/or lateral ligament tear is present. Anterior cruciate ligament surgery can be performed acutely (0-5 days after injury), early (2 weeks), or delayed (6 weeks).
The two most common self-ligament procedures used during anterior cruciate ligament surgery are hamstring tendons and patella tendons (bone-tendon-bone) replacement. In our hospital, we use both procedures as part of minimally invasive arthroscopic surgery.
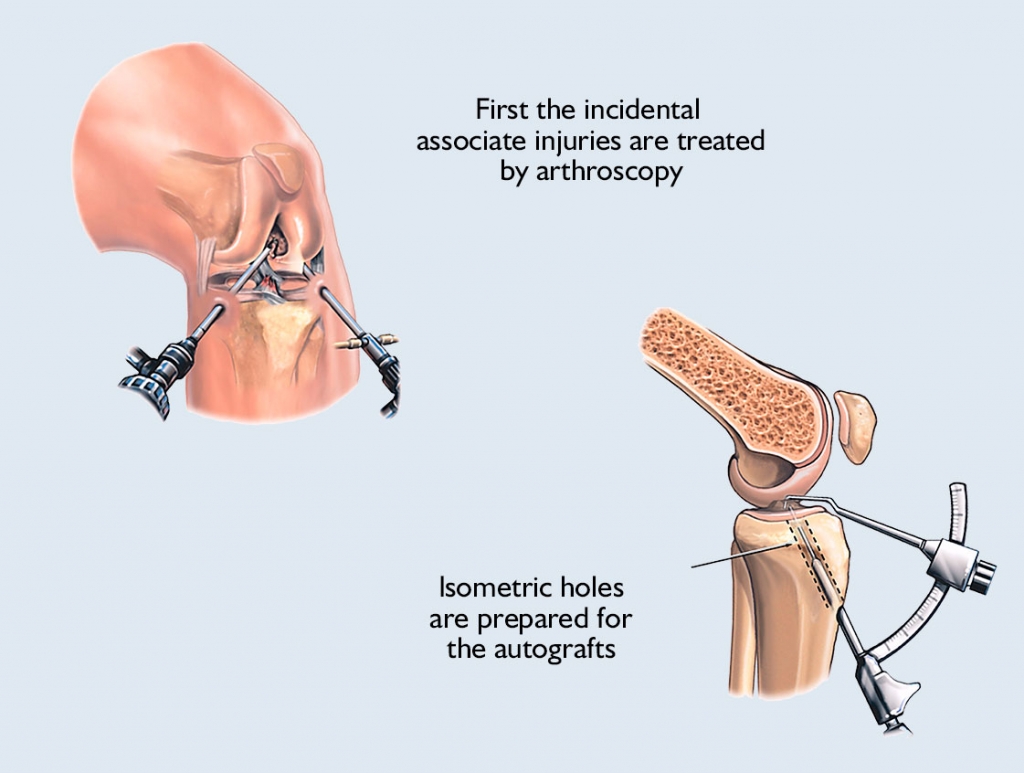
The procedure is performed under general anaesthesia or anaesthesia near the spine. In addition to the kneecap and the kneecap tendon, the knee specialist it makes a half-centimetre incision through which the doctor introduces the arthroscope and the special tools needed for surgery.
The joint is then filled with physiological saline to make the internal structures and lesions to be treated visible. Depending on the finding, any co-injuries are treated first, and then, if all the conditions are met for the replacement of the cruciate ligament, the specialist replaces the torn cruciate ligament using the previously defined procedure.
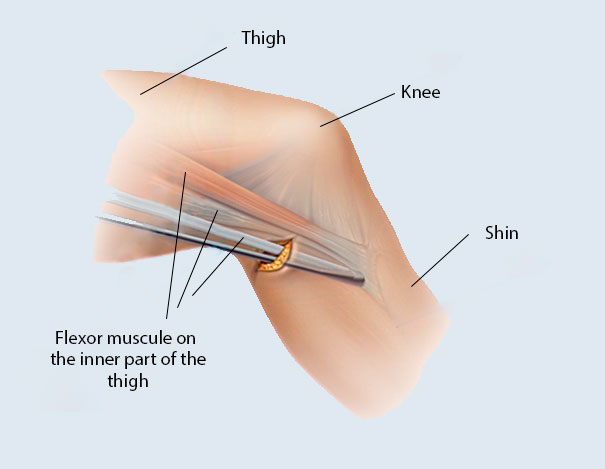
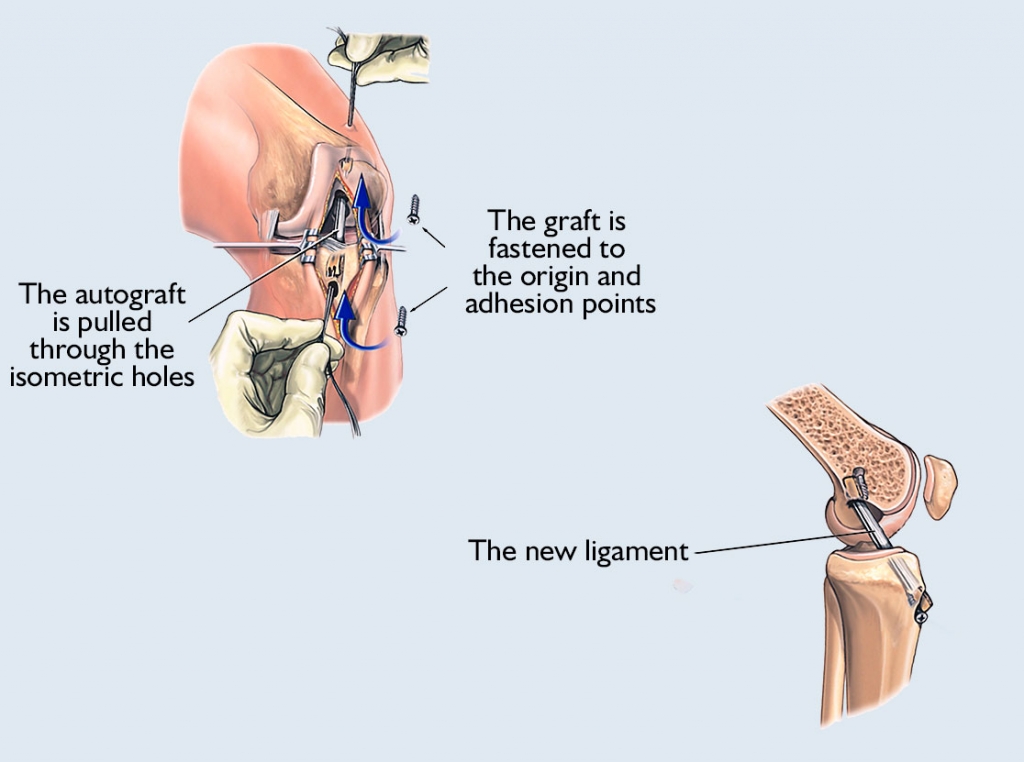
When it comes to the hamstring tendon procedure, the knee specialist looks for the hamstring tendons through a straight incision made on the inside of the part of the leg close to the knee, and then removes the semitendinosus or gracilis tendons with a special device, from which he then makes a graft. The surgeon pulls this graft through the 8-10 mm diameter isometric holes made in the femur and tibia at the original origin and adhesion point of the ligament. The specialist usually secures the graft with a small titanium plate on the femur and a titanium cramp iron on the tibia.
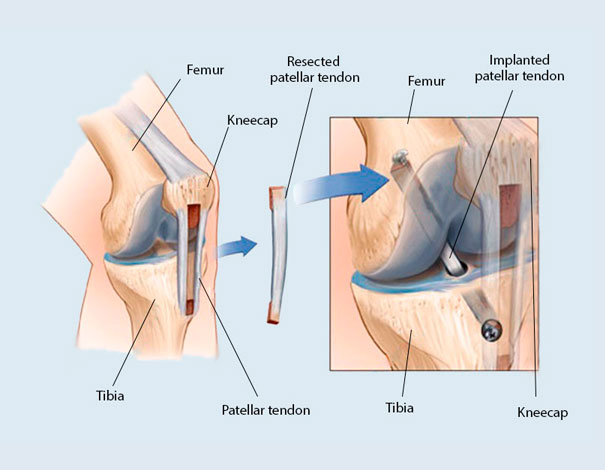
In the patella tendon (bone-tendon-bone) method, the specialist makes an 8-10 cm incision on the anterior surface of the knee joint, through which the middle 1 cm of the 3 cm wide patella is excised, with two bone cubes at the lower and upper ends. The surgeon then implants the ligament arthroscopically: holes are drilled in the femur and tibia through which the doctor pulls the new ligament and secures it with screws.
At the end of the surgery, a suction tube is left in the knee to drain any early haematoma that may form and is usually removed within 24 hours of the surgery.
After anterior cruciate ligament surgery, until wound healing, and in the following few weeks, the use of a long side-rail brace and 3 weeks of relief are required. The day after surgery, conditioning treatment of the thigh muscle begins with physiotherapy, and on day 2 or 3, the patient can leave for home. If no early complication develops, the sutures are removed after 1 week. From the day of surgery until full mobility is achieved, thrombotic prophylaxis is necessary, and the patient is taught how to administer it.
The procedure used to replace the cruciate ligament is chosen by the orthopaedic specialist, taking into account the patient’s age, activity, and degree of injury. Based on research results, a greater degree of stability can be achieved with patella tendon replacement, and in the case of athletes, a larger proportion of patients were able to continue their sports activities like they used to before the surgery.
What aftercare is needed after cruciate ligament surgery?
Anterior cruciate ligament surgery alone does not solve the problem, a stable knee joint also requires professional aftercare. Adherence to the rehabilitation protocol after anterior cruciate ligament replacement is extremely important, as early exercise and exercise with the wrong intensity can lead to damage to the knee joint.
The day after the surgery, the physiotherapist-guided, personalized physiotherapy begins, which the physiotherapist gradually expands with new functions during the healing process. On week 6, after removing the fixation, in addition to performing the extended exercises on a regular basis, cycling is recommended from week 8, and then swimming from week 12.
The patient can return to office work after 4-6 weeks, after 3-4 months to light physical work, and 4-8- months to heavy physical work. Return to active sports after surgery is possible from the 8-10thmonth.
During rehabilitation, other supplementary treatments can be used, such as the PNF (proprio-neuromuscular facilitation) method to increase muscle strength, in which the patient performs static stretching in a passive state with the help of a partner.
What is included in the price of our surgeries?
- costs of the surgery
- costs of anesthesia (local or general anesthesia, postoperative pain relief)
- the costs of the planned hospital stay and care
- necessary medicines and certain medical aids during the stay
- inpatient physiotherapy treatment (if necessary for rehabilitation)
- if necessary, the fee for the planned histological examination
- the price of the first follow-up examination
What additional costs might be expected?
- implants
- consultation with the anesthesiologist (must be done in Medicover)
- pre-operative examinations (if performed by us)
- in case of blood group antibody positivity, the blood matching fee
- hotel service fee for extra care days
- aids for further rehabilitation
- accompanying person staying in the hospital
- day (with one meal) 20 000 HUF
- night (full board) 60 000 HUF
- furthermore, if necessary, the cost of the 2nd follow-up examination is the fee of the specialist examination -50%, the cost of the 3rd follow-up examination is the fee of the specialist examination -30%
The course of the surgery
Before surgery
- pre-surgery specialist consultation, where the specific surgical proposal is made
- consultation with the Case Manager
- general information if necessary
- preparation of a written quotation
- booking surgery and preliminary examination appointments
- payment
-
carrying out pre-operative examinations
-
arrival for surgery
On the day of surgery
- arrival at Medicover Hospital at 6:30
- check-in at the reception on the ground floor
- occupying a room accompanied by a nurse, who provides information
- morning visit with the specialist physician and anesthesiologist
- surgery
- postoperative monitoring
- afternoon visit with the specialist physician
- constant anesthesiology specialist monitoring in the postoperative period
- discharge (with an accompanying person), final report and handing over a certificate
Surgical service process
- surgery
- hospital stay and care
- planned histology
- follow-up examination, sutur removal
