Hand carpal tunnel syndrome surgery, Carpalis tunnel release surgery
Tunnel syndrome surgery, or carpal tunnel release surgery, is an intervention used to treat carpal tunnel syndrome, during which the palm ligament that forms the cover of the “tunnel” is cut through, releasing the nervus medianus from the pressure of the swollen nerves.
What is tunnel syndrome?
Tunnel syndrome is a condition in which the nerves in the holes (“tunnels”) formed by the muscles, ligaments and bones of the body are pressurized, causing numbness or pain in the affected limb.
It can form in the elbow, around the brachial plexus that provides innervation to the arm, in the groin, below the knee, on the dorsum pedis, and most often around the wrist.
How does it develop?
We talk about tunnel syndrome when, for some reason, a narrowing develops next to the descending nerve, which puts pressure on it. Narrowing can also be caused by injury, fracture, inflammation, bone growth, haematoma, tumour, bone or joint developmental disorder.
Swelling of the tendons surrounding the nerve can be caused by several reasons. Some diseases have a much higher risk of developing tunnel syndrome: for example, they may be associated with changes in hormonal balance (hormone-related illnesses, during pregnancy, and with aging) and autoimmune (e.g. diabetes) or other systemic rheumatological diseases.
Most often, a strong, long-term strain can also be the cause of the disease.
It typically affects pregnant and menopausal women, men who are climaxing, and older rheumatic patients.

What are the symptoms of carpal tunnel syndrome?
One of the most common tunnel syndromes is carpal tunnel syndrome at the base of the palm.
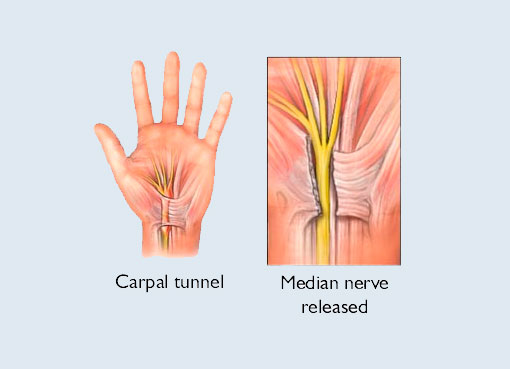
The tendons between the bones of the wrist (carpus), which run in a narrow, tunnel-like hole, swell due to overload or some other reason, squeezing the nerve called the median nerve below them. The nerve medianus, the nerve leading from the cervical spine to the wrist through the shoulder and elbow, which provides innervation for the flexor muscles of the forearm and several hand muscles.
As a result, numbness occurs in the areas covered by this nerve, in the thumb, index, and middle fingers, at first only intermittently, during the day and then at night, and finally this numbness becomes permanent. Increasingly sharp pain, sensory disturbances, tactile numbness occur, and are accompanied by the weakening of the fingers and palms.
The wrist is usually swollen, pressure sensitive, and the pain increases as you move it, especially when you bend it back, often radiating to the forearm and shoulders and neck.
In the advanced state of the disease, due to the pressure on the nerve, the muscles of the palm begin to atrophy, and their grip strength weakens.
It usually develops in the more used, dominant hand.
How is carpal tunnel syndrome diagnosed?
The diagnosis of tunnel syndrome is usually made by an orthopaedic specialist. If there is a suspicion of carpal tunnel syndrome with knowledge of the complaints and medical history, the specialist will perform a specific physical examination to support the diagnosis. If bending the wrist in 90° for a minute or two causes complaints, and when hitting the carpal tunnel, there is an electrifying sensation along the course of the nerve.
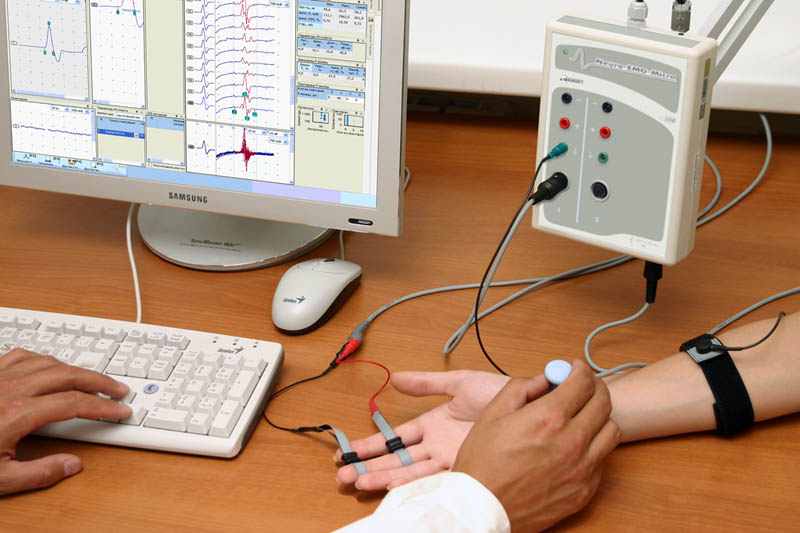
Since tunnel syndromes, such as carpal tunnel syndrome, have similar symptoms as other lesions (e.g. disc herniation, circulatory system diseases), in addition to a physical examination, a special examination, the so-called ENG (electroneurographic) examination is also required. This test measures how fast the peripheral nerves carry the stimulus. The ability of the compressed nerve to conduct stimuli is significantly reduced.
To establish the diagnosis, a neural ultrasound examination may be necessary, as well as an X-ray examination is recommended, which shows the possible bone structure abnormalities and fractures that can lie behind the symptoms.

How to treat carpal tunnel syndrome?
Carpal tunnel syndrome is first treated in a conservative (non-surgical) way. Relieving the hand, stretching the wrist in an extended position at night can reduce swelling within the canal, leaving more space for the nerve. In more severe cases, taking non-steroidal anti-inflammatory drugs in addition, or drugs administered into the carpal tunnel, may also reduce intra-canal swelling.
Surgical treatment of the syndrome by a hand surgeon is also available. Surgery provides the fastest and most effective treatment.
When is surgery warranted?
If conservative treatment is not successful or there is a more than moderate decrease in nerve conduction velocity, a surgical solution is recommended.
What happens during surgery?
During the preoperative consultation our orthopaedist will provide detailed information about the necessary tests before surgery, as well as the course of the surgery and its risks.
The release of the carpal tunnel takes place as part of a one-day surgical procedure.
After surgical preparation, the limb is anesthetized locally. During carpal tunnel release surgery, the pressure on the nerve is relieved by cutting through the palm ligament that forms the top of the canal. During the procedure, the inflammatory tissue proliferation surrounding the tendons is also removed, and the resulting wound is sutured with a few stitches.
The surgery takes only 20 minutes.

What are the dangers of surgery?
As with any medical intervention, the release of the carpal tunnel can have dangers and complications. Very rarely, inflammation and infection of the surgical site, as well as damage to the surrounding anatomical formulas: tendons, muscles, blood vessels, and the median nerve itself, can occur. In such cases, medication may be required in milder cases and repeated surgery in more severe cases.
What can I expect after the surgery?
Sterile, surgical dressings should be replaced the next day. If the dressing is not damaged, no further bandage is required until suture collection without complications. Sutures are removed 10 days after surgery. Gentle exercise for the hands, wrists and fingers is recommended from day 2.
After surgery, scarring around the skin incision may persist for a few weeks, possibly months. Numbness and pain can go away at different rates in the few days after surgery, but it can take months for the handgrip strength to return and the hand to return to its original activity, which can be made faster with a personalized physiotherapy.
What is included in the price of our surgeries?
- costs of the surgery
- costs of anesthesia (local or general anesthesia, postoperative pain relief)
- the costs of the planned hospital stay and care
- necessary medicines and certain medical aids during the stay
- inpatient physiotherapy treatment (if necessary for rehabilitation)
- if necessary, the fee for the planned histological examination
- the price of the first follow-up examination
What additional costs might be expected?
- implants
- consultation with the anesthesiologist (must be done in Medicover)
- pre-operative examinations (if performed by us)
- in case of blood group antibody positivity, the blood matching fee
- hotel service fee for extra care days
- aids for further rehabilitation
- accompanying person staying in the hospital
- day (with one meal) 20 000 HUF
- night (full board) 60 000 HUF
- furthermore, if necessary, the cost of the 2nd follow-up examination is the fee of the specialist examination -50%, the cost of the 3rd follow-up examination is the fee of the specialist examination -30%
The course of the surgery
Before surgery
- pre-surgery specialist consultation, where the specific surgical proposal is made
- consultation with the Case Manager
- general information if necessary
- preparation of a written quotation
- booking surgery and preliminary examination appointments
- payment
-
carrying out pre-operative examinations
-
arrival for surgery
On the day of surgery
- arrival at Medicover Hospital at 6:30
- check-in at the reception on the ground floor
- occupying a room accompanied by a nurse, who provides information
- morning visit with the specialist physician and anesthesiologist
- surgery
- postoperative monitoring
- afternoon visit with the specialist physician
- constant anesthesiology specialist monitoring in the postoperative period
- discharge (with an accompanying person), final report and handing over a certificate
Surgical service process
- surgery
- hospital stay and care
- planned histology
- follow-up examination, sutur removal
