Complete or partial hysterectomy
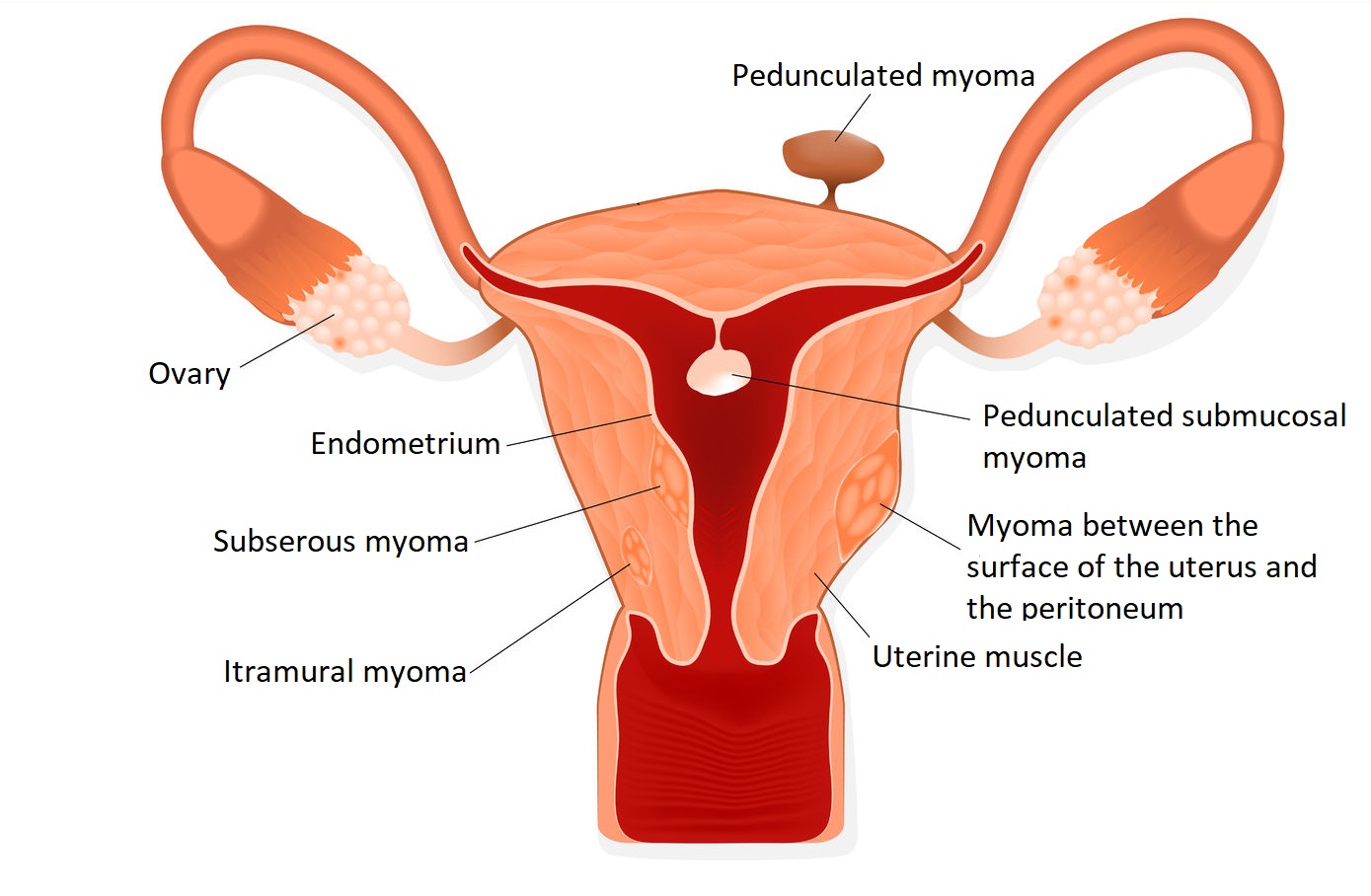
Hysterectomy is a major gynaecological operation in which a patient’s uterus is partially or completely removed. Many diseases can give reason for complete or partial hysterectomy. Most often, in the case of myomas, malignancies, prolapsed uterus, bleeding disorder unresponsive to medication, endometriosis, or pelvic inflammatory disease, your doctor may recommend this procedure.
The surgery is preceded by a thorough gynaecological and ultrasound examination, based on which the specialist determines that abdominal, vaginal or laparoscopic hysterectomy is the appropriate intervention. In some cases, partial hysterectomy is possible, during which the cervix is not removed. In case of patients in perimenopause, removal of adnexa uteri (ovaries and fallopian tubes) is considered.
After hysterectomy, neither menstruation nor pregnancy will not occur. If both sides of the ovaries are removed during surgery, the patient may experience hormone loss symptoms before menopause. The symptoms can be easily eliminated with the help of hormone replacement drugs.
Uterine removal can be done through the vagina, by incising the abdominal wall, or during laparoscopy.
Vaginal hysterectomy
Vaginal surgery is less staining than abdominal hysterectomy, the length of hospital stay is shorter and the healing process is generally faster.
The disadvantage of this procedure is that other abdominal organs cannot be examined during surgery, and prolonged vaginal manipulation can lead to inflammation of the vaginal stump after surgery.
How is vaginal hysterectomy performed?
Surgery can also be performed under spinal anaesthesia or under complete mechanical anaesthesia. After surgical preparation and disinfection, a catheter is inserted into the bladder.
The uterus is removed through the vagina and, if necessary, the vulval vestibule is secured to the ligaments that previously held the uterus. The vaginal wound is closed with stitches. Occasionally, a plastic tube is attached to the wound and removed 1-2 days after surgery. In case of urinary incontinence or vaginal wall prolapse, vaginal wall plastic surgery is performed as well.
If a complication occurs during surgery (e.g. heavy bleeding), abdominal incision may be necessary.
After surgery, drug-relievable abdominal pain may occur, which is later alleviated and then resolved. If there is no complaint, you are usually discharged after 2-3 days.
Avoid sexual intercourse, sitting baths and tampons for 4 weeks after surgery. Contact your doctor immediately if you have fever, bloating or severe lower abdominal pain.
Abdominal hysterectomy
In case of abdominal hysterectomy, the uterus is removed by incision. If the disease only affects the myometrium, the isolated removal of the uterus is possible. In this case, the cervix remains in place and the anatomy of the pelvic floor does not change. The disadvantage of abdominal hysterectomy is the longer healing time due to the invasive nature of the procedure.
How is abdominal hysterectomy performed?
The surgery is performed under anaesthesia through the trachea. After surgical preparation and disinfection, a catheter is inserted into the bladder.
The abdomen is usually opened by a transverse incision, in the line with the pubic hair. For larger lesions, it may be necessary to make an incision in the midline below the navel. The procedure may be supplemented by the removal of the fallopian tubes and ovaries.
Occasionally, it may be necessary to attach a plastic tube to the abdominal cavity, which will be removed the day after surgery.
At the end of the surgery, the abdominal wall wound is joined with sutures. If there is no complaint, you are usually discharged after 2-3 days. Suture collection takes place 7-10 days after surgery. A health conscious lifestyle is recommended for 4 weeks after surgery, with a ban on sitting baths and sexual intercourse.
Laparoscopic hysterectomy
Intervention during laparoscopy is the most modern type of hysterectomy. The advantage of the laparoscopic procedure is that it avoids the conventional opening of the abdomen, which reduces the risks of surgery and speeds up recovery. An ultrasound examination is required before surgery to determine the exact location of the lesions, which helps precise detection during surgery.
How is laparoscopic hysterectomy performed?
The surgery is performed under anaesthesia through the trachea. After surgical preparation and disinfection, a catheter is inserted into the bladder and then a device to move the uterus is attached.
A 1 cm incision is made in the navel and the abdominal cavity is filled with carbon dioxide, and then the laparoscope (orienting optical device) is inserted through the same opening. 2-3 incisions of 5-10 mm each are made above the vulva, through which the microsurgical devices are inserted and the uterus is dismembered and removed.
Occasionally, a plastic tube is inserted into the abdominal cavity, which is removed the day after surgery. At the end of the surgery, the carbon dioxide is released from the abdominal cavity and the incisions are joined by stitching or adhesion.
The patient can get up a few hours after waking up (with the help of a doctor or nurse) and then leave the hospital after a 24-48 hour hospital stay. Suture collection takes place one week after surgery. Avoid sexual intercourse, sitting baths and tampons for 4 weeks after surgery.
What are the risks of hysterectomy?
- Disinfectants and anaesthetics used during surgery can cause an allergic reaction.
- In rare cases, the bladder, urethra and intestinal tract may be damaged.
- Bleeding may occur, which can be alleviated in a hospital setting.
- In case of greater blood loss, blood transfusion may be required.
- Despite the anticoagulant therapy used, thrombosis and embolism may occur rarely.
Risk factors vary from person to person, so be sure to tell your doctor about any previous illnesses, surgeries, surgical complications, and drug susceptibility to minimize the risk of hysterectomy.
What is included in the price of our surgeries?
- costs of the surgery
- costs of anesthesia (local or general anesthesia, postoperative pain relief)
- the costs of the planned hospital stay and care
- necessary medicines and certain medical aids during the stay
- inpatient physiotherapy treatment (if necessary for rehabilitation)
- if necessary, the fee for the planned histological examination
- the price of the first follow-up examination
What additional costs might be expected?
- implants
- consultation with the anesthesiologist (must be done in Medicover)
- pre-operative examinations (if performed by us)
- in case of blood group antibody positivity, the blood matching fee
- hotel service fee for extra care days
- aids for further rehabilitation
- accompanying person staying in the hospital
- day (with one meal) 20 000 HUF
- night (full board) 60 000 HUF
- furthermore, if necessary, the cost of the 2nd follow-up examination is the fee of the specialist examination -50%, the cost of the 3rd follow-up examination is the fee of the specialist examination -30%
The course of the surgery
Before surgery
- pre-surgery specialist consultation, where the specific surgical proposal is made
- consultation with the Case Manager
- general information if necessary
- preparation of a written quotation
- booking surgery and preliminary examination appointments
- payment
-
carrying out pre-operative examinations
-
arrival for surgery
On the day of surgery
- arrival at Medicover Hospital at 6:30
- check-in at the reception on the ground floor
- occupying a room accompanied by a nurse, who provides information
- morning visit with the specialist physician and anesthesiologist
- surgery
- postoperative monitoring
- afternoon visit with the specialist physician
- constant anesthesiology specialist monitoring in the postoperative period
- discharge (with an accompanying person), final report and handing over a certificate
Surgical service process
- surgery
- hospital stay and care
- planned histology
- follow-up examination, sutur removal
