PCOS (polycystic ovary syndrome) laboratory test package
Performing our PCOS laboratory package tests is recommended if polycystic ovary syndrome is suspected. The laboratory tests included in the package will help diagnose the syndrome.
What is PCOS?
PCOS stands for polycystic ovary syndrome (or Stein – Leventhal syndrome), which covers not only the ovaries but the whole body. In addition to genetic predisposition, lifestyle (overweight, stress, sedentary lifestyle) is an important factor in the development of metabolic disorders affecting the female hormonal system. Nowadays, its occurrence is very common, affecting about 5-7% of women.
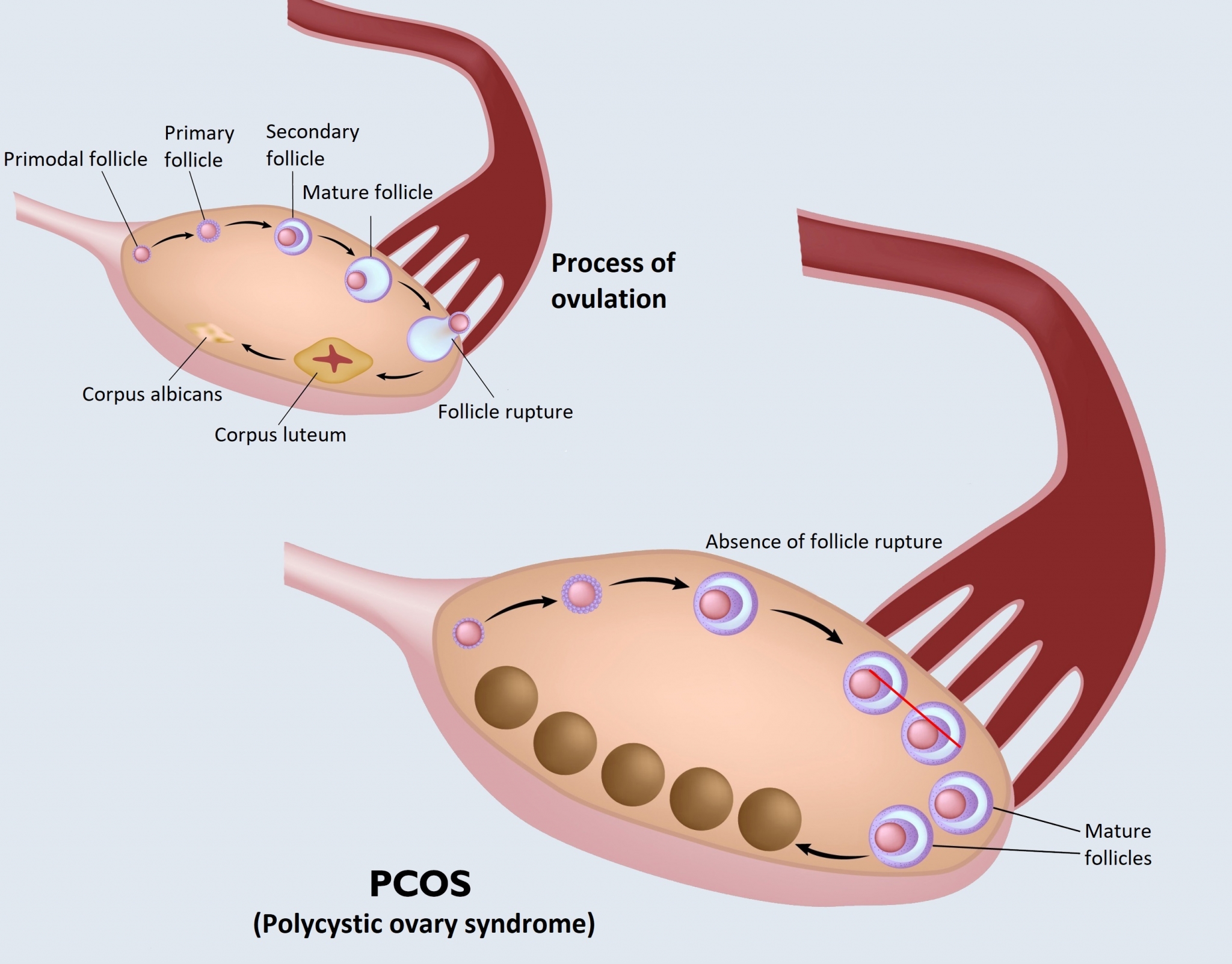
The cause of the syndrome is the predominance of steroid hormones (male sex hormone). The predominance of androgenic hormone in the female body is associated with menstrual disorders, increased hair growth, and acne prone skin. A capsule forms on the surface of the ovaries, which prevents the rupture of follicles (ovulation). The uncracked follicles thus remain in the ovaries, forming tiny cysts that become visible in a shape similar to beads on the ultrasound image.
The syndrome is often accompanied by insulin resistance and diabetes, as these conditions can trigger a number of additional hormonal and metabolic changes in the body. Ovarian and adrenal disorders increase the production of androgenic hormones (testosterone, DHEA-S, androstenedione), luteinizing hormone (LH), and at the same time reduce the secretion of progesterone and follicle stimulating hormone (FSH), which can be clearly detected with the laboratory test package.
What symptoms may indicate PCOS?
PCOS can cause both internal medicinal, gynaecological complaints, and skin problems. It does not have uniformly characteristic symptoms, it usually causes different complaints at each stage of life, in a “composition” that varies from individual to individual.
Common symptoms include acne, oily skin, brown discolouration of the neck or armpits, severe hair growth on the face and body due to the predominance of male hormones, baldness and thinning hair, obesity around the abdomen, and after meals, sudden tiredness or tremor, irregular or missing menstrual cycle, or infertility.
When is it recommended to perform the PCOS laboratory package?
If PCOS is suspected, it is advisable to consult an endocrinologist, but gynaecological and internal medical tests are also required for diagnosis. The examination continues after exploring the complaints and physical examination (body weight, waist and hip circumference measurement, body mass index determination, blood pressure measurement) with laboratory tests included in the PCOS laboratory package, as well as abdominal and vaginal ultrasound examinations. The latter can be used to detect the presence of uncracked follicles in the ovaries and the thickening of the endometrium caused by the absence of menstruation.
PCOS can be considered if the tests confirm the presence of at least two of the following 3 main symptoms:
- Irregular menstruation or ovulation disorder
- Male hormone overweight
- Ultrasound shows tiny cysts under the ovarian cortex
What tests does the PCOS package include?
The PCOS laboratory package includes testing for female and male sex hormones, monitoring thyroid function and vitamin D levels, and a 3-point oral glucose tolerance test combined with insulin measurement.
Total and free testosterone: an androgenic hormone produced in the ovaries and adrenal glands in women. An increase in free testosterone levels may occur with normal total testosterone levels. As a result of its increased value, masculine features appear (thick body hair, masculine baldness), which may also be due to PCOS.
Prolactin: The hormone prolactin helps initiate and maintain milk secretion after childbirth. In addition to pregnancy, low and high levels may indicate PCOS, among other things.
Oestradiol: A type of oestrogen hormone produced by the maturing follicle. The determination of oestradiol levels is primarily used to test ovarian function. A lower value may also indicate PCOS.
Androstenedione: an androgenic hormone produced in women by the ovaries and adrenal cortex. Its level varies during the menstrual cycle, helping to monitor ovarian function. In the case of PCOS, its level is increased.
DHEA-S: androgenic hormone, which in women can be converted into female sex hormone, oestrogen. Its high level causes amenorrhea (absence of menstruation) and masculinity. Elevated values are also characteristic of PCOS.

Progesterone: plays an important role in the formation and maintenance of pregnancy but is also partly responsible for the regulation of the female menstrual cycle. Its concentration also indicates whether a follicular rupture has occurred.
AMH (anti-Müllerian hormone): produced by eggs that are still maturing, so the expected length of the fertility period can be deduced from its level. As the years go by, its level gradually decreases. AMH is significantly elevated in PCOS, preventing early follicular maturation.
FSH (follicle-stimulating hormone, follicle maturation hormone): FSH initiates the growth and development of follicles in the ovaries. By determining its level, we can get information about the function of the ovaries, in case of PCOS, its value is normal or decreased.
LH (luteinizing hormone, corpus luteum stimulating hormone): LH triggers ovulation (follicular rupture). It further matures the follicle prepared by FSH; when LH levels increase, ovulation occurs. By determining its level, we can get information about the function of the ovaries, its elevated value indicates insufficiency. In case of PCOS, the normal 1:1 LH:FSH ratio shifts in favour of LH.
Thyroid function
TSH: We examine the levels of the thyroid-stimulating hormone, TSH , which is produced in the pituitary gland and stimulates thyroid hormone production. In case of PCOS, TSH levels are usually elevated and the thyroid gland has decreased function.
Metabolism
3-point oral glucose tolerance test with insulin measurement: In addition to consuming a solution containing 75g of glucose, an oral glucose tolerance test is performed, in parallel with which the insulin level, the degree of secretion and its change are measured. With PCOS, blood sugar levels and insulin levels are also elevated.
Vitamin D: Vitamin D plays a role similar to hormones in the development and maturation of eggs. In case of PCOS, its levels are low, which can also affect the intensity of the symptoms that occur.
How do I prepare for the test?
Sampling takes place at two times.
The first sampling happens between days 3-5 of menstruation (days 3 to 5 from the start of bleeding). This is when most hormone tests (AMH, FSH, LH, testosterone, prolactin, oestradiol, androstenedione, DHEA), thyroid function and vitamin D levels, as well as oral glucose tolerance and blood sugar tests are performed. The glucose tolerance test means 3 samples on this day: one on an empty stomach and then one at 60 and 120 minutes after consuming the glucose-containing fluid. It is recommended that a diet of 150 grams of carbohydrate be maintained for at least 3 days prior to the test, and a 12-hour fast is required for fasting blood sampling prior to the test.
The second sampling takes place on day 21 of menstruation, at which time progesterone levels are monitored. It is no longer necessary to arrive with an empty stomach for this sampling.
When is the result expected?
The test results of the first sampling will be available on the 17th working day after sampling. The results of the second sampling will be uploaded to our online system on the 3rd working day after the sampling.

What to do after the test?
The obtained result does not in itself constitute a diagnosis; in order to make an accurate diagnosis, always consult your doctor or the specialist who ordered the examination.
The symptoms of polycystic ovary syndrome can be successfully treated, and treatment can also prevent complications such as type 2 diabetes, high blood pressure, or infertility. In many cases, lifestyle changes (healthy eating, diet, regular exercise) also contribute to the cessation of certain symptoms. The required treatment plan is determined by an endocrinologist with the involvement of a gynaecologist, internal medicine specialist or dietitian as needed. The syndrome requires constant monitoring to prevent the recurrence of symptoms.
