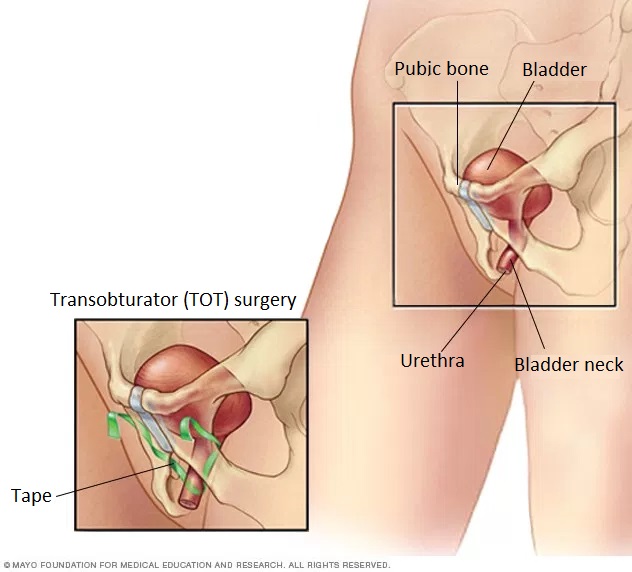
Anti-incontinence (TOT – Transobturator tape) surgery
What is incontinence?
Urethral urinary incontinence can be mild, moderate, and severe. According to its types, we distinguish between stress incontinence, urge incontinence, overflow incontinence, and reflex incontinence.
When is anti-incontinence (TOT) surgery necessary?
TOT surgery can be used to completely or partially eliminate a form of urine dripping, called stress incontinence (loss of urine due to pressure on the abdomen, strain), if conservative treatment methods fail.
How is TOT surgery performed?
Anti-incontinence surgery can be performed under anaesthesia or near spinal anaesthesia. The surgery is performed with the legs raised, in the so-called lithotomy position.
In the first step, a catheter is inserted into the bladder to drain the urine. Then, under the urethral opening, approx. a 2cm incision is made on the anterior vaginal wall. A passage is made on both sides of the urethra to the obturator foramen (oval or irregular triangular opening in the hip bone) on the pubic bone.
Then, in the crotch, approx. a 1–5 mm skin incision is made 2–3 cm above the urinary meatus, and then a special skewer is inserted from the outside through this skin incision to pierce the membrane of the obturator foramen. The skewer is lead between the bladder and the vagina until the end of the skewer is pushed out at the vaginal wall incision.
The end of the tissue-friendly plastic tape, which has been developed for this purpose, is then fastened to the end of the skewer and the tape is pulled in with the skewer, the end of which is outside the skin in the crotch. This operation is performed on both the right and left sides.
At the end of the anti-incontinence surgery, the tape is fixed under the urethra without straining, as shown in the figure. The protruding parts of the tape are cut off on both sides, and then the vaginal wall wound and crotch wounds are closed with absorbable suture. A long cloth soaked in braunol is placed in the vagina.
The morning after the surgery, the longetta in the vagina and bladder catheter are removed. After the first spontaneous urination, the fullness of the bladder is checked with ultrasound. If there is no urine left, the patient can be discharged.
What are the benefits of TOT surgery?
The advantage of anti-incontinence surgery is the effective, causal treatment of the disease. The efficiency of TOT surgery is 80-85% considering the whole continence, i.e. the elimination of urinary dripping is fully achieved in such a percentage.
What are the risks of TOT surgery?
The frequency of complications is negligible compared to the number of surgeries performed. After TOT surgery, a so-called urge symptom (de novo urge symptom) may occur, which can result in the patient experiencing sudden urination stimuli. This condition may resolve temporarily and spontaneously, but medication may also be required. Bleeding, tape rejection, or urethral, vaginal, or bladder corrosion by the ligament may occur after the procedure.
How do I prepare for the surgery?
The attending physician explains the reason that necessitates anti-incontinence surgery and summarizes the essence of the intervention. The procedure can be performed under anaesthesia or near spinal anaesthesia. If your doctor has prescribed medication before anti-incontinence surgery, you should take it at the specified time.

What to do after anti-incontinence surgery?
After the procedure, mild pain may occur in the affected surgical area, which in some cases may be accompanied by bruising in the crotch area covering the skin incision. There may be little bleeding from the vaginal wound. The dressing covering the surgical wounds should initially be protected from moisture. Suture collection is not necessary, the stitches are completely absorbed in 4-6 weeks. Medication should be used as directed by a doctor to prevent infections and reduce pain.
The patient can leave the hospital on the 2nd day after anti-incontinence surgery.
Convenience services
We accommodate our clients in a modern, pleasant, air-conditioned single room. Each room has a private bathroom, fridge and TV, as well as free WIFI access. We also provide our clients with individual nurse supervision, who will help your continuous recovery during your stay.
What is included in the price of our surgeries?
- costs of the surgery
- costs of anesthesia (local or general anesthesia, postoperative pain relief)
- the costs of the planned hospital stay and care
- necessary medicines and certain medical aids during the stay
- inpatient physiotherapy treatment (if necessary for rehabilitation)
- if necessary, the fee for the planned histological examination
- the price of the first follow-up examination
What additional costs might be expected?
- implants
- consultation with the anesthesiologist (must be done in Medicover)
- pre-operative examinations (if performed by us)
- in case of blood group antibody positivity, the blood matching fee
- hotel service fee for extra care days
- aids for further rehabilitation
- accompanying person staying in the hospital
- day (with one meal) 20 000 HUF
- night (full board) 60 000 HUF
- furthermore, if necessary, the cost of the 2nd follow-up examination is the fee of the specialist examination -50%, the cost of the 3rd follow-up examination is the fee of the specialist examination -30%
The course of the surgery
Before surgery
- pre-surgery specialist consultation, where the specific surgical proposal is made
- consultation with the Case Manager
- general information if necessary
- preparation of a written quotation
- booking surgery and preliminary examination appointments
- payment
-
carrying out pre-operative examinations
-
arrival for surgery
On the day of surgery
- arrival at Medicover Hospital at 6:30
- check-in at the reception on the ground floor
- occupying a room accompanied by a nurse, who provides information
- morning visit with the specialist physician and anesthesiologist
- surgery
- postoperative monitoring
- afternoon visit with the specialist physician
- constant anesthesiology specialist monitoring in the postoperative period
- discharge (with an accompanying person), final report and handing over a certificate
Surgical service process
- surgery
- hospital stay and care
- planned histology
- follow-up examination, sutur removal
