Urology
Urology and the urologist deal with congenital and acquired disorders and diseases of the urinary tract (kidney, ureter, bladder, urethra). These include developmental anomalies, infections, inflammation, lithiasis, urinary discomfort – difficulty urinating, involuntary urination – and cancer. Additionally, the urologist also examines and treats the problems of the male genitals (testicles, prostate, penis).
The course of the urological examination
Most examinations focus on screening for prostate cancer and diagnosing benign prostatic hyperplasia. Bacterial and abacterial chronic prostatitis are common in younger men. In case of patients with complaints and various symptoms, the anamnesis is especially important to get to know the possible medical history, diseases occurring in the family, and the general condition of the patient. This is followed by a general urological examination.
Our experienced urologists working in our Clinics will receive you with the greatest discretion.

With what symptoms should you see a urologist?
It is recommended to visit a urologist with the following symptoms:
- Frequent, painful, pungent, bloody urination
- Urinary incontinence
In case of men:
- Difficult, intermittent urination
- Decreased urine output, nocturnal urination
- Sexual dysfunction (erectile dysfunction)
The most common urological examinations
Investigation of urination complaints
Observable symptoms such as frequent urination, urinary retention, bloody ejaculation, urinary or urethral bleeding are typical of a later stage, so regular urological examination is essential for early detection and effective treatment of the disease.
Impaired bladder emptying leads to the insufficient contraction of the bladder muscle. Bladder emptying disorder is diagnosed with a functional diagnostic tool. The urine flow test provides evaluable information about the characteristics of urination using the amount of urine, the average and maximum rate of urination, and a urination curve. During the test, the patient empties his bladder into a funnel-shaped container attached to a measuring instrument. The measurement can be evaluated if a minimum of 150 ml of urine is excreted.
Investigation of problems caused by prostatic hyperplasia
Due to the enlargement of the prostate, the patient’s urine is starting difficultly and is intermittent in a thin stream. Urination involves exertion, with a minimal amount of urine being excreted. The urge to urinate occurs very frequently. Other symptoms include incontinence and cystitis due to urinary retention or bacterial superinfection. A more serious complication may be the inability to urinate, which develops when the enlarged prostate compresses, thus blocking the first section of the urethra.
For men who experience pain when urinating as well as a thick urge to urinate, a prostate laboratory test is recommended to look for problems caused by prostate enlargement.
Screening for prostate cancer
Prostate cancer is the most common cancer in men, which mostly occurs at old age. In the early stages of prostate cancer, when it can still be successfully treated, it is often completely asymptomatic, so it is extremely important that men from the at-risk age (45 years) have a urological examination every year.
During the rectal digital examination, also known as prostate examination, the specialist will feel the prostate gland through the rectum. If a tumour is suspected due to the hardness and size of the tissue, the texture and sensitivity of the prostate, further examination is required. These include ultrasound examination of the prostate through the rectum (transrectal examination), measurement of PSA levels by blood sampling, CT examination, and tissue sampling (biopsy).
During prostate biopsy, ultrasound-guided needle puncture sampling is performed from both lobes of the prostate through the rectum.
Ultrasound-reflecting ability of tumour tissue is weaker than that of healthy tissue, so abnormal tissue appears as a black spot on ultrasound examination. The so-called PSA is a protein produced by the glands of the prostate. It is true that PSA levels in the blood are significantly elevated in case of prostate cancer, but this also occurs in other non-neoplastic diseases of the prostate, so a definitive diagnosis can only be made after a histologic examination.
Testicular cancer
Testicular cancer is a rare cancer that occurs more often in the younger age group. Screening is based on home self-examination. We recommend palpation of both testicles once a month. If the patient experiences an abnormality, during the urological examination, it will be diagnosed by physical examination, followed by testicular ultrasound and the necessary laboratory tests.
Investigation of acute and chronic urinary tract infections
Urinary tract infection is one of the most common infections, mostly of bacterial origin, in which the pathogens that cause the infection enter the bladder through the urethra. The sedentation of pathogens results in inflammation of the tissues. Infection can result in lower urinary tract infection called urethritis, or cystitis. The development of complications depends on how far the pathogens go. In more severe cases, an upper urinary tract infection, i.e., pyelitis, can also develop.
The diagnosis of a urinary tract infection is made based on symptoms, by urinary and blood tests, and by examination of the urinary tract and kidneys.
Urinary continence problems
Urethral urinary incontinence can be mild, moderate, or severe. In some cases, a thorough examination of the patients includes a urodynamic test, which can also reveal the cause of the incontinence. If conservative treatment methods do not lead to results, the procedure used to eliminate stress incontinence (loss of urine due to exertion) completely or partially, is called the TOT surgery.
Kidney stone
The kidney is a paired, bean-shaped organ responsible for excretion. Its function is to remove metabolic breakdown products, filter and purify the blood, and regulate the body’s water balance.
Kidney stones form in the urinary tract and drainage organs when the balance between fluid and solutes is upset.
Initially, only tiny crystals are form, which are stacked in several layers, and if they do not leave the urinary system for a long time, they turn into stones, which in most cases are yellow or brown.
The most common symptoms are sharp, stabbing, or cramping pain, back pain, bloody urine, nausea/vomiting, and bloating.
Genetic predisposition, inadequate fluid intake, one-sided diet, sedentary lifestyle, urinary tract infection, and urinary retention may all underlie kidney stone formation.
In addition to the presence of known symptoms, abdominal ultrasound, CT urography, and laboratory examination of renal function are of great importance in making the diagnosis.
Types of kidney stones
More than twenty types of kidney stones (calcium stone, oxalate stone, uric acid stone, cystine stone, struvite stone, etc.) are known. The main component is predominantly calcium oxalate, to a lesser extent, calcium phosphate. Yellow or brown stones can range in size from sand grains to fist-sized. An individualized dietary recommendation tailored to the type of stone can be made after a urine test and stone analysis.
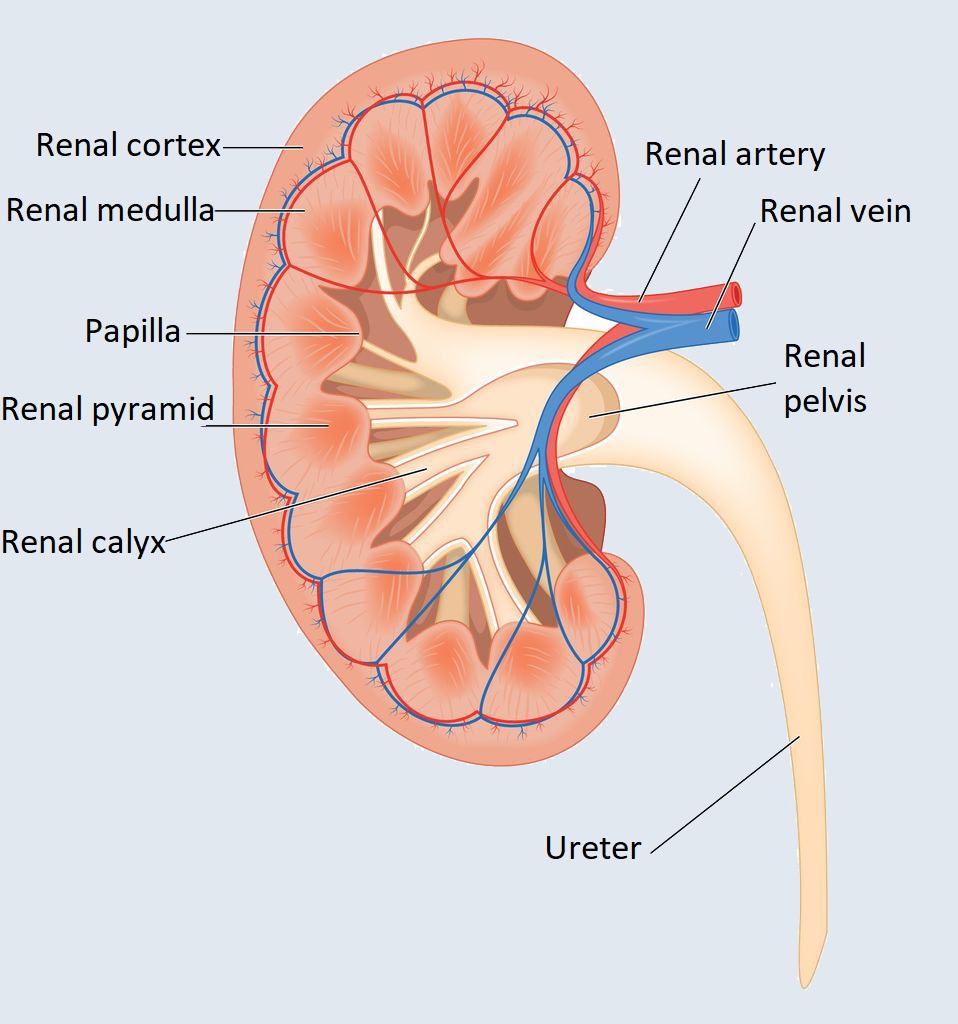
Structure and function of the kidney
The kidney is a bean-shaped, paired organ located at the back, on either side of the spine, at about waist height. Their size is 12 cm x 4 cm and they weigh approx. 140 grams each.
The surface of the kidneys of a healthy adult are smooth and bright brown. It is surrounded by a three-layer connective tissue case on the outside.
The kidneys are responsible for excretion, removal of the breakdown products that are formed during metabolism, filtering and purifying the blood, and regulating the body’s water balance and arterial blood pressure.
It also removes certain foreign substances – xenobiotics – that enter the body, the end products of nitrogen metabolism (creatinine, uric acid, urea) and some inactivated hormones, as well as drugs.
If the concentration of normal metabolic products exceeds the required – physiological – value, these products (glucose, lactic acid, ketone bodies) are also excreted by the kidneys.
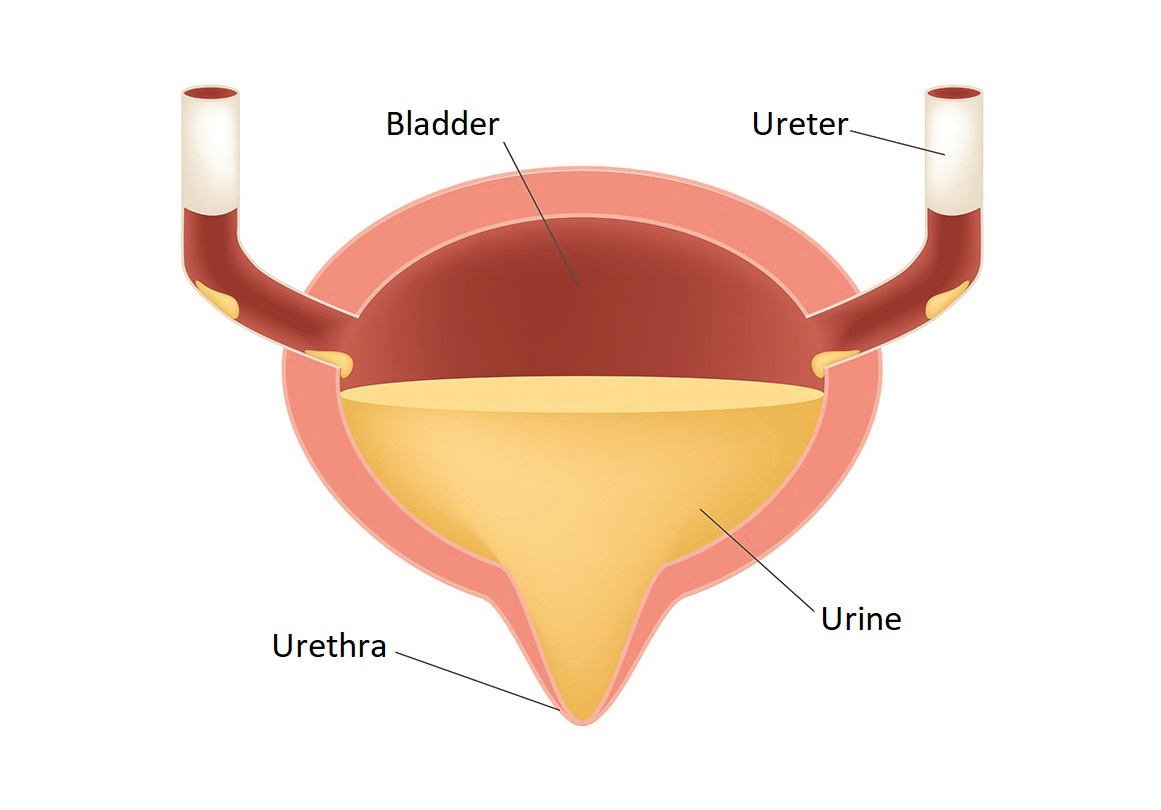
Structure of the bladder
The bladder is a hollow organ with a muscular wall lined with mucous membranes for storing urine. It is located in the lesser pelvis. It is connected to the prostate in men and to the front wall of the vagina in women. Its posterior surface is covered by the peritoneum. It has three openings for the two ureters as well as the urethra.
From the kidneys, urine enters the bladder through the ureters, which, thanks to its multi-layered epithelium and muscular wall, is also able to adapt to larger volume changes. The urination stimulus occurs when the urine accumulated in the bladder reaches a volume of 300-350 ml. Urine leaves the bladder through the urethra. The sphincter around the urethral opening can be opened or closed voluntarily.
Function and structure of the testicles
The testicles are male gonads that produce sperm and male sex hormones – testosterone. They are located in the scrotum. Next to them are the epididymis, which consist of winding canals and store sperm. The testicles in the embryo begin to develop in the abdominal cavity and then descend to the perineum-area. The blood supply of the testicles starts directly from the aorta. Blood continues to flow in the spermatic cord until it reaches the testicles.
The testicles are surrounded by a connective tissue sheath and are composed of canals. Spermatozoon is produced in these winding canals. The testicular ducts are made up of germinal epithelium. The testicular ducts contain Sertolli cells, in which the sperm cells undergo a maturation process and take up nutrients. The so-called Leydig cells between the testicles are responsible for the production of testosterone, which plays an essential role in the development of secondary sex (body shape, height, sound, etc.).
The epididymis is attached to the posterior surface of the testicles. It consists of a head, a body, and a tail. Its substance is made up of epididymal canals. Sperm production no longer takes place here, they are just stored.
The spermatic cord is a muscular-walled tube starting from the tail of the epididymis. Going upwards in the scrotum, it enters the abdominal cavity through the inguinal canal. Spreading downward behind the bladder, it opens like a semen ejection canal into the urethral section of the prostate gland.
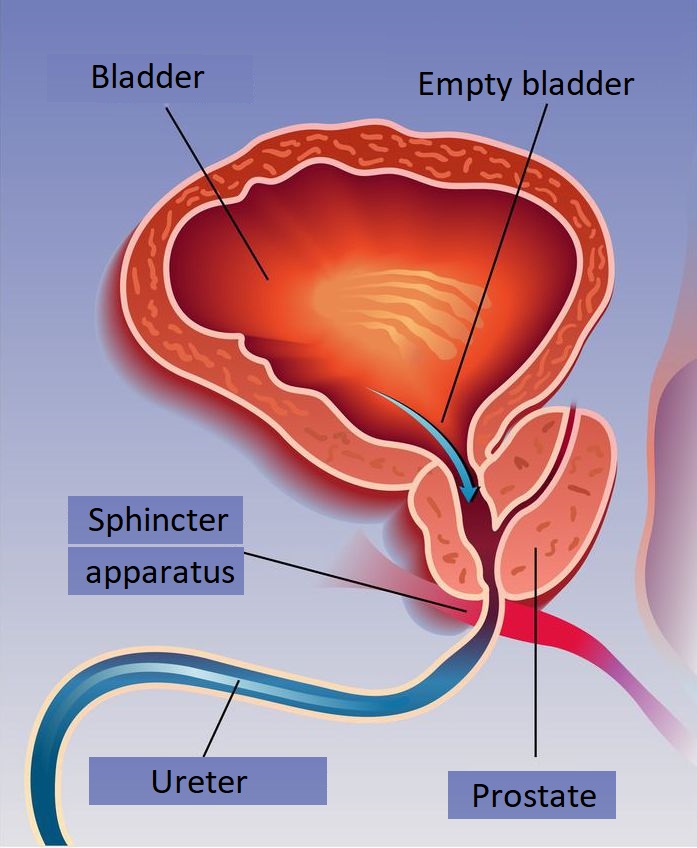
Function and structure of the prostate
The prostate (prostate gland) is a gland that belongs to the male genitals. The prostate in healthy adult men weighs 20-25g, is about the size of a chestnut, but can enlarge in old age due to hormonal changes.
The most common diseases of the organ are benign prostatic hyperplasia, prostatitis, and malignancies.
It is located just below the bladder, surrounding the first section of the urethra. The outlet tube of the prostate glands of the prostate opens into the urethra, as do the spermatic cords.
When it comes to its structure, the prostate is made up of glands surrounded by muscle tissue, which is surrounded by albuginea. The movement of the smooth muscle that makes up the prostate plays a role in urination and ejaculation.
Prostate secretions produced in the glands, together with sperm cells and seminal vesicle secretions, form the male genital secretions, the semen.
The main function of prostate secretion is to help the movement of sperm and, thanks to its alkaline pH, to neutralize the acidic pH of the female vagina for the viability of sperm.
